Getting you back to work and life in Thornton & Broomfield, CO
Lumbar (Low Back) & Cervical (Neck) Spine
More than 90 percent of Americans will suffer from debilitating low back/neck pain at some point in their lives. Getting you back to work and the activities that you enjoy as quickly as possible is our goal at the Center for Spine and Orthopedics.
Our diverse team of highly experienced spine and pain management specialists offer a wide range of nonsurgical and surgical treatment, from spinal injections, acupuncture and neural blocks to minimally invasive spine surgery, spinal fusion and artificial disc replacement. While we recognize that 80 percent of patients receive relief without surgery, we are committed to providing the safest, highest quality surgical procedures possible when surgery is necessary to relieve pain. Learn about the surgical procedures we offer below (or click on Pain Management to learn more about our non-surgical treatments).

We offer a wide range of nonsurgical and surgical treatments
Lower Back (Lumbar Spine)
Surgical Treatment Options

Although an estimated 70 to 80 percent of people experience low back pain at some point in their lives, most do not need surgery to relieve their pain. The time to consider surgery is when low back pain does not improve with conservative treatment.
What are the surgical options for treating lower back pain?
a. Lumbar spine fusion (arthrodesis) is the most common surgical option for treating low back pain when nonsurgical treatment does not relieve back pain. Spinal fusion eliminates motion between vertebrae and prevents the stretching of nerves and surrounding ligaments and muscles. It is an option when motion is the source of pain, such as the movement that occurs in a part of the spine that is arthritic. The theory is if the painful vertebrae do not move, they will not hurt.
While lumbar fusion helps many patients, others do not improve. Some surgeons believe this is because fusion prevents normal motion in the spine. Though fusion takes away some spinal flexibility, most spinal fusions involve only small segments of the spine and do not limit motion very much.
b. Artificial disk replacement (ADR) is an alternative to spinal fusion for lower back pain. Not all patients that are candidates for spinal fusion are candidates for artificial disc replacement. However, all candidates for ADR are candidates for spinal fusion (arthrodesis).
General considerations for artificial disc replacement are:
- Back pain caused by one or two problematic intervertebral discs in the lumbar (low back) spine
- No significant facet joint disease or bony compression on the spinal nerves
- Significantly overweight
- No major lumbar surgeries
- No significant spinal deformity (scoliosis)
- Normal quality bone
What is involved in artificial disk replacement for the lumbar (lower back) spine?
Artificial disk replacement involves removing worn or damaged disk material between the vertebrae and replacing it with a synthetic or “artificial” disk. The materials used for ADR are very similar to total knee and total hip replacements.
The goal is to relieve back pain while maintaining more normal motion than with other procedures, such as spinal fusion (arthrodesis). This procedure generally takes two to three hours. As with fusion, not all patients improve with ADR.
What are the types of lumbar (low back) spinal fusion (arthrodesis)?
There are several different techniques and approaches that your surgeon can use to fuse the spine, including an:
- Anterior approach, when your surgeon approaches your spine from the front. This is called anterior lumbar interbody fusion and requires an incision in the lower abdomen.
- Posterior approach, which is done from your back and called a posterior lumbar interbody fusion
- Lateral approach, when your surgeon approaches your spine from the side. This is called lateral interbody fusion.
- Minimally invasive techniques, which allow fusions to be performed with smaller incisions.
The surgical goal is the same with all of these procedures—fusion of the involved vertebrae. The right procedure for you depends on the nature and location of your particular anatomy and disease process.
What can you expect after surgery for artificial disc replacement (ADR) and lumbar (lower back) fusion?
In most cases, you will stay in the hospital for one to three days after your surgery, depending on your pain and return to function. Most patients are encouraged to walk by the first day after surgery. Depending on your pain, you may start a form physical therapy program shortly after surgery.
The postoperative rehabilitation program will vary somewhat, depending on your specific condition, your general physical conditioning before surgery and whether you have had a fusion (arthrodesis) or an ADR.
Most patients’ lower back pain improves in weeks to months after their surgery. However, disk replacement, as with spinal fusion (arthrodesis) may not completely eliminate pai
Some other advanced surgical terms you may you may hear about from other patients or read about in the newspaper relate to Minimally Invasive Surgery. Minimally Invasive Spine Surgery (MISS) is a surgical procedure that is performed through several small incisions (usually less than one inch) rather than through a five- to 10-inch incision with traditional “open surgery,” thus avoiding significant damage to the muscles surrounding the spine. With MISS, doctors use specialized instruments to access the spine through small incisions. Faster recovery, less postoperative pain, a shorter hospital stay, less bleeding, and a more cosmetic approach to incisional scars are some of the benefits of minimally invasive surgery. Patients are also less likely to develop complications.
Minimally invasive techniques have been used for common procedures, such as decompression and spinal fusion, since the 1990s, and they are beginning to be used for a wider range of back and neck procedures. Although MISS holds advantages for many patients, some back and neck problems cannot yet be treated effectively with minimally invasive methods.
Remember that the goal of MISS is the same as with larger incisions; only the approach is somewhat different.
Microsurgery is a type of minimally invasive surgery, using an operating microscope and specially designed surgical instruments. The microscope enables surgeons to perform delicate operations through an incision as small as 1 to 1.5 inches in length.
The new advances using an operating microscope for smaller incisions have enabled anterior (frontal) approaches to thoracic and lumbar spine surgery. Anterior exposure of the lumbar spine can be very effective in biopsy and fusion procedures. In the anterior approach, the lumbar spine may be exposed through a two- to four-inch incision in the abdomen, allowing the surgeon to pass through the abdomen or shift the abdomen structure to expose the spine. These approaches are called Transabdominal and Retroperitoneal respectively.
New techniques in posterior spinal surgery have led to smaller incisions, making it possible to provide outpatient spine surgery with minimal muscular disruption and faster recovery times.
Additionally, the use of minimally invasive surgery techniques have allowed conditions, such as scoliosis (curvature of the spine), kyphosis (hump back), fractures, and tumors which may require major surgical procedures from two approaches: anterior and posterior to occur simultaneously. Today, surgeons can use minimally invasive surgery techniques to work on the front and back, in many cases eliminating the need for two separate surgeries. This approach has proven to be safer, result in fewer complications, allow quicker recovery, and be more cost effective than traditional surgical approaches.
Not all procedures are amenable to minimally invasive techniques, but these new advances have provided a greater range of surgical options for spine patients.
How are fusions and decompression procedures performed with MISS for lumbar (low back) pain?
MISS fusions and decompression procedures, such as a discectomy and laminectomy, are performed with special tools called tubular retractors. During the procedure, your surgeon will make a small incision and then insert the tubular retractor through the skin and soft tissues down to the spinal column. This creates a tunnel to the small area where the problem exists in the spine. The tubular retractor holds the muscles open and stays in place throughout the procedure.
Your physician then accesses the spine using small instruments that fit through the center of the tubular retractor. Any removed bone or disk material exits through the retractor, and any devices necessary for fusion — such as screws or rods — are inserted through the retractor. Some surgeries require more than one retractor.
To see where to place the incision and insert the retractor, your surgeon is guided by fluoroscopy, which displays real-time x-ray images of your spine on a screen throughout the surgery. The surgeon also uses an operating microscope to magnify the view through the retractor. It provides excellent illumination and magnification during minimally invasive spine procedures.
At the end of the procedure, the tubular retractor is removed, and the muscles return to original position. This limits the muscle damage that is more common during open surgeries.
What are the most common minimally invasive spine surgeries?
Minimally invasive lumbar (low back) discectomy and minimally invasive lumbar (low back) fusion are two of the most common MISS procedures.
How is a minimally invasive lumbar discectomy performed?
Essentially, this is a decompressive procedure to relieve pain caused by a damaged disc pressing on the nerve in your lower back, causing severe leg pain, numbness or weakness. Your physician will remove part or all of your damaged (herniated) disc to relieve your pain.
To perform this procedure, the surgeon will make a small incision (usually less than one inch) over the damaged (herniated) disk as the patient lies facedown. Then, he or she will insert the retractor and remove a small amount of the lamina bone. This enables the surgeon to view the spinal nerve and the disk. Then, the physician carefully removes the damaged disk and replaces it with bone graft material.
This minimally invasive technique can also be used for herniated disks in the neck. The procedure is done through the back of the neck and called an MIS posterior cervical discectomy.
How is minimally invasive lumbar fusion (arthrodesis) performed?
Minimally invasive lumbar fusions can be performed from the back, through the abdomen or from the side.
Transforaminal lumbar interbody fusion (TLIF) is a common type of MISS fusion. With this technique, the surgeon approaches the spine a little bit from the side, reducing how much the spinal nerve must be moved. In an MIS TLIF, the surgeon places one retractor on either side of the spine while the patient lies facedown. This approach prevents disruption of the midline ligaments and bone. Using the two retractors, the surgeon can remove the lamina and the disk, place the bone graft into the disk space, and place screws or rods to provide additional support.
Minimally invasive spinal fusion is also commonly performed from the side. There are two procedures that use a side approach: extreme lateral interbody fusion (XLIF) and direct lateral interbody fusion (DLIF). The benefits of lateral fusion surgeries are that they do not injure the back muscles or pull on the nerves in the spinal canal.
What are the benefits of minimally invasive procedures?
MISS patients typically go home in two to three days, depending upon the procedure. Because minimally invasive techniques do not disrupt muscles and soft tissues, postoperative pain is usually less than with traditional, open procedures.
How long does it take to recover from MISS?
How long it will take to return to your daily activities after MISS depends on your procedure and condition. To help speed your recovery, your doctor may recommend physical therapy. Specific exercises will help you become strong enough to return to work and daily activities.
If you have had a fusion procedure, it may be several months before the bone is solid, although your comfort level will often improve much faster. Your doctor will evaluate you after surgery to make sure that your recovery is progressing as expected.
Lumbar (low back) herniated disc microsurgery enables a surgeon to use an operating microscope and special small instruments to remove the ruptured disc material associated with a herniated disc from the spinal canal. Most patients leave the hospital within eight to 12 hours with significant less pain.
Lumbar (low back) Spinal stenosis microsurgery – With spinal stenosis, resulting from degeneration and arthritis, microsurgery can remove bone or tissue that has thickened, narrowing the spinal canal and impacting nerve function. By relieving the pressure on the spinal nerves via microscopic removal of the damaging bone or tissue, severe pain, numbness, weakness, bowel and bladder problems, and in severe cases, partial paralysis can be eliminated or improved. Most patients leave the hospital within 24 hours.
Understanding Back & Neck Fractures
Other Conditions Of The Spine

When cervical radiculopathy (a pinched nerve in the neck) persists or worsens despite nonsurgical treatment, your physician may recommend surgery. The primary goal is to relieve pressure on the compressed nerves in your neck. Other surgical goals include reducing neck pain; maintaining your spine’s stability; improving spinal alignment; and preserving your neck’s range of motion.
Surgery for a pinched nerve in your neck usually involves removing pieces of bone and/or soft tissue (such as a herniated disk). This relieves pressure by creating more space for the nerves to exit the spinal canal.
What are the most common surgical options for treating cervical (neck) radiculopathy?
The three most common surgical options are:
- Anterior cervical diskectomy and fusion (ACDF)
- Artificial disk replacement (ADR)
- Posterior cervical laminoforaminotomy
The procedure your surgeon recommends depends on your problem and its location; your overall health and medical history; and your preferences.
What is anterior cervical (neck) discectomy and fusion (ACDF)?
ACDF is the most commonly performed procedure to treat a pinched nerve (cervical radiculopathy). It involves removing the problematic disk or bone spurs and then stabilizing the spine through spinal fusion.
With an “anterior” approach, your surgeon will approach your neck from the front. He or she will operate through a one- to two-inch incision along your neck crease. During your procedure, your surgeon will remove the problematic disk and any additional bone spurs if needed. The disk space will be restored to its height before the disk wore out, making more room for the nerves to leave the spine and aiding decompression.
After the disk space has been cleared out, your surgeon will use fusion to stabilize your spine. Fusion eliminates motion between the degenerated vertebrae and decreases some spinal flexibility; the theory is that if the painful spine segments cannot move, they will not hurt.
What is involved with cervical (neck) artificial disc replacement (ADR) surgery?
Cervical ADR is a breakthrough procedure that restores range of motion and offers significant relief for spinal pain associated with cervical disc degeneration. It involves removing the degenerated disc and replacing it with artificial parts, as with hip or knee replacement. The goal of disc replacement is to allow the spinal segment to keep some flexibility and maintain more normal motion than is seen with spinal fusion.
Similar to ACDF, your surgeon will use an “anterior” approach for the surgery—making a 1- to 2-inch incision along the neck crease. The exact location and length of your incision may vary depending on your specific condition.
During the surgery, your surgeon will remove your problematic disc and then insert an artificial disc implant into the disc space. The implant is made of all metal or metal and plastic. It is designed to maintain the motion between the vertebrae after the degenerated disc has been removed. The implant may help restore the height between the vertebrae and widen the passageway for the nerve roots to exit the spinal canal. Remember that a candidate for a ADR is always a candidate for fusion, but a candidate for fusion may not be a candidate for ADR.
Although no longer considered a new technology, the development of ADR is more recent than ACDF. To date, the outcomes of ADR surgery are promising and are comparable to that of ACDF surgery. ADR may be an option for you, depending on the type and location of your problem. Your doctor will discuss options with you.
What is involved with a posterior cervical laminoforaminotomy?
Unlike ACDF, posterior cervical (neck) laminoforaminotomy does not require spinal fusion to stabilize the spine. Thus, you will maintain better range of motion in your neck, and your recovery will be quicker.
During a posterior cervical laminoforaminotomy, your surgeon will make a one- to two-inch incision along the midline of the back (posterior) of your neck and then use specialized tools to thin down the bony arch that forms the backside of the spinal canal (lamina). Removing this allows your physician better access to the damaged nerve. He or she then removes the bone, bone spurs and tissues compressing the nerve root. If your compression is due to a herniated disk, your doctor will also remove the part of the disk compressing the nerve.
What can you expect after surgery for any of these three options?
After surgery, your hospital stay will usually last one or two days. Most patients are able to walk and eat on the first day after surgery. You may need to wear a soft or a rigid cervical (neck) collar for a length of time at first, depending on your surgeon’s recommendations.
Shortly after surgery, your physician may recommend only light activity, like walking. As you regain strength, you will be able to slowly increase your activity level. Usually by 4 to 6 weeks, you can gradually begin to do range-of-motion and strengthening exercises. Some surgeons start range of motion exercises within a week of surgery. Your physician may also prescribe physical therapy to help you regain full function.
Most patients are able to return to a desk job within a few days to a few weeks after surgery. They may be able to return to full activities by three to four months, depending on the procedure. For some people, healing may take longer. With spinal fusion, it may take from six to 12 months for the bone to become solid.
Most patients experience favorable outcomes after cervical radiculopathy surgery. They usually experience pain relief and are able to return to daily activities after a recovery period.
Degenerative Disc Disease (Arthritis/Spondylosis) Procedures for the Neck (Cervical Spine) and Low Back (Lumbar Spine)
Summary Of Surgical Options
 Regardless of the approach—traditional ACDF MISS or posterior surgery with/without fusion (arthrodesis)—the major goal of these surgeries is to decompress the neural structure(s) that is (are) compressed. Adding fusion (arthrodesis) or artificial disc is based on your specific case.
Regardless of the approach—traditional ACDF MISS or posterior surgery with/without fusion (arthrodesis)—the major goal of these surgeries is to decompress the neural structure(s) that is (are) compressed. Adding fusion (arthrodesis) or artificial disc is based on your specific case.
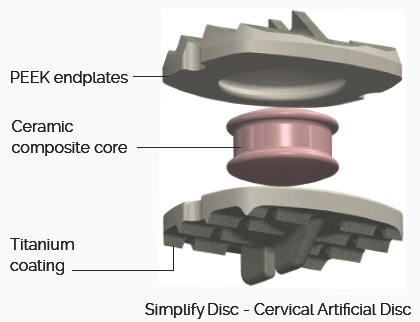
Are you experiencing numbness, tingling or pain in your neck, shoulder or arm? Simplify Disc is a cervical artificial disc that may be of interest to you.
Simplify® Disc is an investigational device designed to:
- Permit the full diagnostic imaging capability of MRI
- Minimize patient exposure to ionizing radiation from CT scans
- Be available in disc heights as low as 4mm to treat a broad range of patients
You must meet certain criteria to take part in Simplify® Trial:
- Age 18-60
- Diagnosis of cervical radiculopathy or myelopathy requiring treatment at one level
- Failure to respond to non-surgical treatment
- Ability to attend follow-up progress visits over a 24 month period and probably longer
For more information, please contact Dr. Michael Janssen’s research assistant, Ruth Beckham, NP-C, at 303.287.2800, ext. 323 or email beckhamr@centerforspineandortho.com.
In general, for back pain only, when surgery is indicated, lumbar (low back) fusion (arthrodesis) is an indicated procedure between the offending vertebrae(s).
Whether your surgeon performs anterior (front) lumbar interbody fusion or posterior (low back) interbody fusion or lateral (side) interbody fusion depends on your specific case. Your surgeon will discuss these details with you. When equally effective methods exists, your surgeon will also review these with you.
Artificial disc replacement between the offending vertebrae(s) is an alternative to fusion (arthrodesis). In some cases, the approach will be anterior (front, through the abdomen).
If your case only involves only nerve issues (radiculopathy) with little or not low back pain, i.e. herniated nucleous pulposis (HNP), the objective is decompression of the offending nerve structures. This can be accomplished posteriorly (low back) by using a traditional approach or with MISS (with or without microsurgery).
If your case involves lumbar (low back) pain and lower extremity pain (radiculopathy), your surgeon will review variations of these options with you. Usually, he or she will use a combination of decompression of the offending nerve(s) along with spinal (lumbar) fusion or artificial disc replacement.
Decompression is a surgical procedure for relieving pressure and alleviating pain caused by an impingement. A small portion of the bone over the nerve root, called lamina, and/or disc material from under the nerve root is removed to give the nerve more space.
There are three common types of spinal decompression procedures, all of which can be done using minimally invasive techniques:
- Laminotomy/foraminotomy – shaving off part of the lamina to create a larger opening to relieve the pinched nerve.
- Laminectomy – Complete removal of the lamina.
- Discectomy – Removal of part of a disc that is compressing a nerve.